Biochemical genetics
There is considerable research strength in the area of Biochemical Genetics at the Manchester Children’s Hospital in collaboration with the University of Manchester. Three groups actively collaborate to deliver a bench-to-bedside approach to the diagnosis, research and development and treatment of a range of metabolic and lysosomal diseases, including mucopolysaccharide diseases, for which Manchester is the leading centre for research and treatment in Europe.
The team is made up of the:
- Willink Biochemical Genetics Unit: the clinical arm under Dr Simon Jones
- Blood and Marrow Transplant Unit under Dr Rob Wynn (consultant haematologist)
Basic and early translational research in these areas is coordinated in the MPS Stem Cell Research Laboratory under Dr Brian Bigger.
What are lysosomal storage diseases?
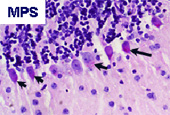
Lysosomal storage disorders (LSDs) and related metabolic diseases are individually rare, but have a cumulative incidence of approximately 1 in 7000 live births. Many of these diseases occur through genetic deficiencies in lysosomal enzymes, resulting in accumulation of undegraded substrates within lysosomes of the cell. Examples of disease include mucopolysaccharide (MPS) diseases, such as Hurler Syndrome (MPS I) and Sanfilippo syndrome (MPS III) storing glycosaminoglycans; Sphingolipid storage disorders such as Tay-Sach’s, Fabry and Gaucher disease, and many others. Although substrates accumulated are quite variable, many of these disorders affect the central nervous system of children, resulting in severe progressive neuronal decline, visceral organ enlargement and dysfunction and bone and joint disease in some cases. Severe forms of disease, which are the predominant manifestation, usually result in death in early childhood.
How can metabolic diseases be treated?
Treatment modalities for LSDs are very limited and represent a clear unmet clinical need. Aside from palliative management of disease symptoms, they consist of three main options in clinical practice today:
- Enzyme replacement therapy (ERT) is partially effective at managing milder forms of disease. Replacement enzyme delivered to the plasma can be taken up by mannose or mannose 6 phosphate receptors present on the surface of most cells and transported to the lysosome where it becomes active, a phenomenon known as cross correction. However, barriers to enzyme bioavailability, including the blood brain barrier and relatively avascular sites, such as the growth plates of the bone, preclude effective distribution of enzyme to sites of clinical need in severe forms of disease, thus severely limiting the use of this therapy. ERT is costly, as weekly injections are required to maintain enzyme levels and this and its inability to cross the blood brain barrier, limit ERT treatment to non-neuronopathic Gaucher, mild forms of MPSI, II, VI and Fabry.
- Substrate reducing drugs such as NB-DNJ have proven to be partly effective in diseases such as late onset Gaucher disease, A clinical trial in Niemann Pick C disease has also suggested efficacy on CNS symptoms although not in all patients treated. No effective substrate reducing agents have yet been discovered for mucopolysaccharide diseases.
- Haematopoietic stem cell transplantation (HSCT), is the only curative therapy in current use for a very small subset of LSDs and is thought to function by bone marrow derived microglial cells trafficking into the brain and providing enzyme for cross-correction. In severe forms of MPS I, bone marrow transplantation provides a significant correction of the neurological phenotype in affected patients, although bony disorders are less well corrected. In other disorders, such as Krabbe, MPS III and Metachromatic Leukodystrophy, no clear neurological improvement is noted in patients following transplantation and although visceral organs are apparently corrected and some slight delay in appearance of neurological symptoms may occur, neurodegeneration is not significantly altered.