Clinical case study: Infection
Scenario
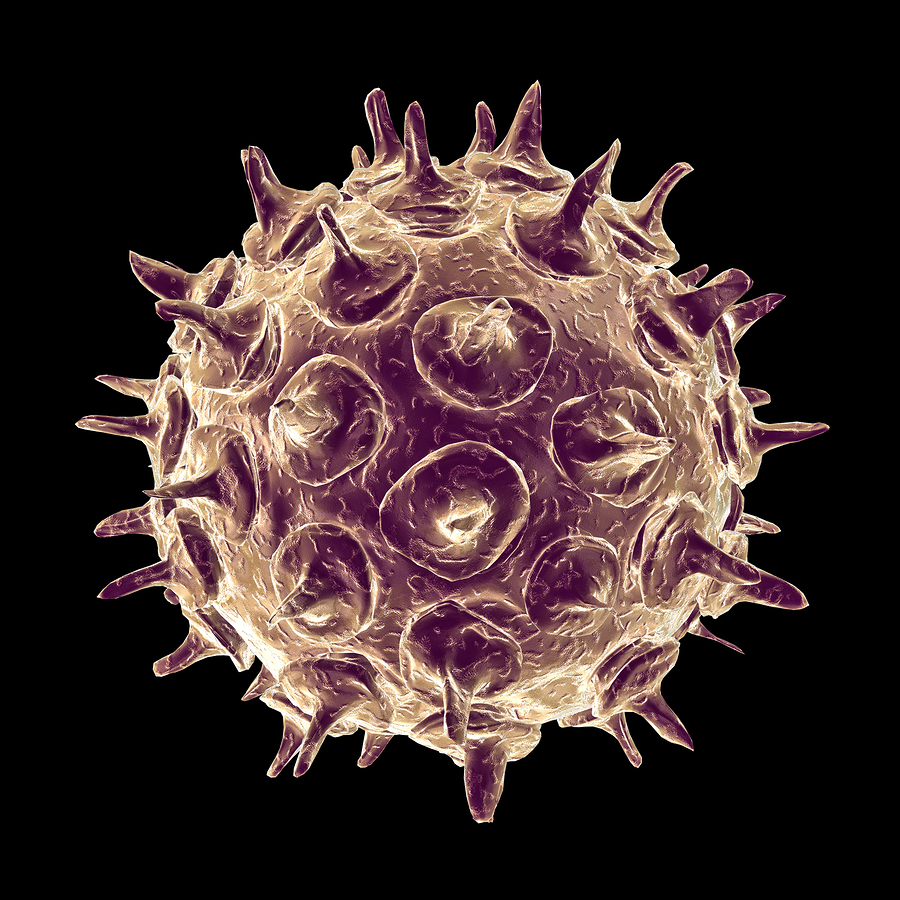
Image source: https://microbewiki.kenyon.edu/
Dr Lomax is a staff grade anaesthetist working in the NHS at a District General Hospital. She presents to the Occupational Health department after talking to her consultant, as she has noticed recent symptoms which she feels are affecting her work. You see her in your capacity as an occupational health physician within the Trust.
The consultation
The history
She complains of general malaise together with a rash. Further questioning reveals that she has noticed mild "flu like" symptoms for about three days. On the day she presents to the occupational health department she notices that a rash has appeared on her face. There is no other significant current or past medical history and she is not taking any medication.
On examination
She has a few vesicles on her face, which she says have appeared that day. The distribution and appearance of the rash leads to her being diagnosed as having chicken pox. Dr Lomax cannot remember having chicken pox in the past.
The Occupational Health staff have taken a blood sample to test for antibodies and sent her home pending the result.
What work-related information would you need to obtain from Dr Lomax?
- Where (specifically) in the Trust she was working for the 2 days prior to the appearance of her rash
- Whom she has been in contact with (staff and patients) over this time period - note that contact is defined as being in the same room for 15 minutes or more, or having a face-to face-conversation with another individual.
Clinical effects of infection with varicella
Varicella is a viral infection which can affect children and adults and infection in adults is likely to be severe. Patients are infectious for 2 days prior to appearance of the rash, until the vesicles have healed.
What do you know about transmission rates for varicella?
Varicella is highly transmissible and secondary transmission rates can be as high as 90% in close contacts.
Which groups of patients might be more susceptible to the effects of varicella?
Immune suppressed and neonates are highly susceptible to severe disease and may die of the illness.
What do you know about the syndrome associated with varicella infection during the first 20 weeks of pregnancy?
This may result in limb hypoplasia, microcephaly, cataracts, growth retardation, skin scarring and interuterine death.
Risk assessment
In Dr Lomax's case, as a staff grade anaesthetist she may have been highly mobile throughout the hospital. She may well have worked on the delivery suite, resuscitated a neonate, or worked on ITU in the past few days. Non-immune individuals who have been in contact with her need to be identified.
Human varicella-zoster immunoglobulin can be given to vulnerable individuals to provide protection if the patients are identified in time. Non-immune health care workers are potentially infectious from day 11 to day 21 from the date of contact and should be suspended from clinical duties during this period (note that there may be local policies and national guidance on periods of infectivity which may not reflect the timescale quoted here).
Immunology
You requested urgent blood tests for varicella IgG which come back the same day. These are negative and show that Dr Lomax is not immune to varicella. The diagnosis should be assumed to be varicella until you have the varicella IgM results, which will not be available for 3 days.
What additional information about Dr Lomax might be of importance with respect to her diagnosis?
An important issue to take into consideration would be Dr Lomax's country of origin. If she came from a region where varicella infection in childhood was rare (for example the Asian sub-continent) then this, along with the clinical history, should also support you keeping to your diagnosis of varicella - pending the awaited results.
Further actions
With the information currently available to you, what would you do at this stage?
- You will need to let the Control of Infection department know about this possible index case. They will liaise with the Dr Lomax's doctors and arrange appropriate testing and treatment
- Dr Lomax needs to know that she will remain infectious until she has no new crops of vesicles and any existing vesicles have crusted over
- You will now need to trace all identified staff contacts to see if their records show them to be immune to varicella
- Those who are immune may stay at work; those known not to be immune must refrain from clinical duties from day 11 to day 21 from the date of contact with Dr Lomax
- Staff whose immunity is unknown and with no history of chickenpox must be tested for varicella zoster IgG. The results from this are usually available fairly quickly (4 hours) but this may vary locally. Any decisions as to whether these staff should go off work pending results will depend on your individual risk assessment of the circumstances.
Preventative measures
Any non-immune staff could be offered immunisation.
- The chickenpox vaccine is not part of the routine childhood vaccination schedule in the UK. The vaccine is currently only offered on the NHS to people who are in close contact with someone who is particularly vulnerable to chickenpox or its complications. There is a licensed, safe and effective vaccination available privately
- In recent years it has been used as part of the routine childhood vaccination programme in the USA
- Licensing of this vaccination in the UK and official guidance on its use is detailed in Chapter 34 of Immunisation against infectious disease - 'The Green Book'
- Occupational Health use of the vaccine as described above is a licensed indication
- In the UK the government now offers routine vaccinations to people aged 70 years old to provide protection against shingles and to introduce a catch-up immunisation programme for people aged 79 years.
Cost benefit analysis
You might like to perform a cost benefit analysis (or risk assessment) of vaccination of the non-immune staff in a hospital using the following figures:
- Cost of the vaccine = varies but is currently between £65 and £100
- Maximum proportion of staff you would find to be non-immune = 10%
- Against this, you should set the likely financial cost to a hospital of keeping staff away from work (as in this example).
Further reading
- CDC: Preventing Varicella in Health Care Settings.
- Department of Health: Immunisation against infectious disease - 'The Green Book'.
