Case study 1: Dizzy and deaf
Introduction
This lady has had a standard work-up for investigating dizziness associated with deafness. There are a number of different medical "takes" on this sort of issue which will come up as sub-themes or complications from time to time. In this particular type of case, one such theme is likely to be occupational. How might such an element come up?
- In the medical history?
- From clinical investigations?
Historically, noise from work has been a common cause of deafness but occupations noisy enough to cause significant deafness in a 40-year old woman are now quite rare. That is still not the case though for your 60 or 70 year old patients where the possibility must be much nearer to the front of your mind from work they may have done 40 or 50 years earlier.
In fact, the greater risk to your 40 year old patient may be inappropriate or incautious attribution to noise. Thus individuals who work in call centres, which is now a very common job, quite often complain of auditory effects associated with work. However, the volume of communication can be adjusted, whereas the noise from leisure activities tends to be uncontrolled or adjusted upwards (e.g. concerts and portable media players).
In these circumstances, they may experience a phenomenon called "temporary threshold shift (THS)" which can carry over into work. THS is basically a defence mechanism to protect the ear whereby, to some extent, the sensitivity of hearing is "shut down" when exposed to higher levels of noise. It may take several hours to recover - it can be demonstrated on audiograms.
Another set of considerations may need to be brought into play if your 40 year old patient is a recent immigrant, especially from a developing country. Many women may well have worked from childhood in a noisy industry, especially the clothes trades, where the older machinery often used is very noisy indeed. Similar circumstances can also be found in sweatshops far nearer than might be expected (and hoped)!
Finally, it is worth noting, as work-associated noise-induced deafness becomes more unusual, smaller rather specific sub-sets of workers become more prominent as being at risk. Amongst these are former military personnel and firearms officers.
Comment
If this lady had presented to you, you might have sent her for investigation to an ENT clinic or to a neurologist. How do you think going down one investigation route rather than another might have affected how your patient was dealt with?
Along a similar line of thinking, supposing she had presented initially in an OH clinic rather than in a GP surgery?
Theoretically, where you start and where you end up in a medical process should depend on need and so the outcome should be the same. But even if you are thinking about the patient holistically then it may still be that “holistic” means different things to different people. In the occupational health clinic, the patient would certainly be directed towards investigation of the complaints that she had reported, usually through her GP. However the occupational health approach would also be to assess and adapt to any problems she might have with doing her work. A GP might be more likely to advise the patient to refrain from work pending investigation.
- Is one of these approaches more holistic than the other?
- Why might there be conflicts about these approaches?
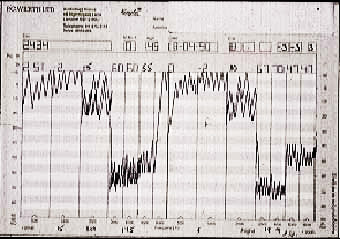
Diagnostically, noise-induced effects, whether they be temporary threshold shifts or permanent noise-induced deafness, are relatively easily and precisely identifiable. Typically noise produces a so-called “dip” in the audiogram centred on the zone round 4000Hz (see the image above). This may be superadded to other conditions, including age-related effects.
ENT clinics are well-used to making the diagnosis of noise-induced hearing loss (NIHL).
- If the lady had what you suspected to be NIHL, might she be eligible for compensation?
- How would you temper your advice to avoid unduly raising her expectations with regard to compensation?
