
THOR-GP
The Health and Occupation Research network in General Practice
THOR-GP collects data on patients with occupational disease seen by approximately 200 GPs with training in occupational medicine.
This scheme allows us to build a picture of occupational disease and will include patients who do not have access to occupational health providers through their workplace. Like OPRA, the scheme incorporates all categories of work-related ill health.
THOR-GP has been operating at the COEH in The University of Manchester since 2005.
Reported diseases
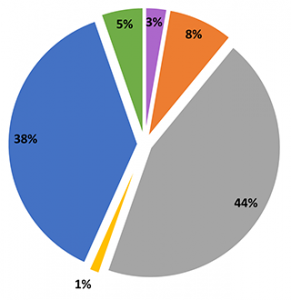 A total of 1,888 cases were reported to THOR-GP between 2010 and 2019:
A total of 1,888 cases were reported to THOR-GP between 2010 and 2019:
- Musculoskeletal – 44%
- Mental ill health – 38%
- Skin – 8%
- Other occupational disease – 5%
- Respiratory – 3%
- Audiological – 1%
Who can join THOR-GP?
To become a THOR-GP reporter, you must be a UK based general practitioner with a formal qualification in occupational medicine (D Occ Med, AFOM or MFOM), and/or have undertaken an approved DOccMed training course (e.g. CPD in Occupational Medicine at the University of Manchester).
Reporting your data
Reporters to the THOR-GP scheme report for one randomly allocated month per year.
You must only report cases seen in your general practice clinic. Please see our full clinical guidelines here. To find out more about how to report using our online reporting system please see our reporting guidelines here.
Online reporting of occupational cases is done via a secure web form. You will have your own account for completing this form.
You will receive a reporting email, which includes your username and password, at the beginning of your randomly allocated month.
“This is a new area of information collection in occupational health and I felt it needed support. I have found it instructive and that it takes very little time or effort.”
Dr J Lubin / General Practitioner
Blogs by our reporters
You can read blog posts by current THOR-GP reporters about their experiences on the THOR blog.
Join THOR-GP now
To join us as a THOR-GP reporter, please complete our recruitment form.
Contact us
If you have any questions about THOR-GP, please contact George McHale:
Current reporters
If you have already joined this scheme, you can access your reporting form by logging into the THOR Reporting Site.
